Key Resources for Junior Doctors returning to training
We’ve put together the best resources out there to support you with return to medical training. Be as active as possible in planning both your time away and the course of your return – you, your patients and those you may go on to mentor will thank you for it!
General resources
The Gold Guide
Download the latest (7th – published 2017) edition of The Gold Guide to stay up to date with leave and return policy.
HEE’s Supported Return To Training
Ensuring returning to training is as smooth as possible is a major priority for Health Education England and suggestions for support are being responded to – as you can see from this report. Though not created to signpost to existing services, it is well worth a read to reassure you that your misgivings about a return are shared and also keep you in the loop as to what services may be expanding into your Deanery soon.
Tea and Empathy
This Facebook Group is a national, peer-to-peer support network specifically designed for NHS practitioners, though is also accessible to any other medical practitioner. Discussions here capture all aspects of training – good times and bad. This site allows for anonymous posting via administrators and includes closed regional groups. Peer-to-peer support can be offered through private messenger and is completely confidential.
The Royal Medical Benevolent Fund
This organisation provides a variety of opportunities to obtain and provide support for doctors in training or currently practicing. This website specialises in both emotion-focused and problem-focused support, providing opportunities to receive psychological care, financial support and advice on a range of topics. This site is by far the most pragmatic available with resources on everything from how to handle a difficult landlord to considering whether an alternative career might be right for you. Content here is produced by medical professionals from all specialisms and levels of seniority – you’re certain to find something relevant to you.
Junior Doctors’ Terms and Conditions of service
Like the Gold Guide, this provides exhaustive information on expectations regarding leave and return.
Headspace
This app (mostly free of charge though subscription options are available) provides detailed guides on how to make mindfulness work for you-you may find their pain and stress management guides particularly useful. Headspace has been demystifying mindfulness for millions of subscribers and for a price of just 10 minutes a day, you have so much to gain in terms of mental resilience and effective stress-management, even in the most difficult of circumstances. If right for you, Headspace stands as an opportunity for you to explore and strengthen your stress response both during and after your leave.
Parental Leave
Medical Women’s Federation
Provides detailed information on how best to navigate returning to work after giving birth. Tips here are pretty exhaustive but again emphasise the need to be proactive in arranging for support.
BMA information sheet on Working Parents
This is an exhaustive guide to how to plan and manage the demands of balancing being a parent with being a trainee practitioner both before and after your child is born. This includes useful resources including a Maternity Leave checklist and calculator and information on shared parental leave and how best to return to training.
BMA information sheet on Paternity Leave
This provides a comprehensive view of paternity entitlements and how to go about notifying your Deanery.
BMA information sheet on Maternity Leave
This provides a detailed view of maternity entitlements and how to go about notifying your Deanery. It also provides contact information for personalised advice.
BMA information sheet on Parental Leave
This source outlines eligibility, time allowances for leave, notification requirements from parents and how to handle unreasonable refusal of leave requests.
Government Information On Parental Leave
Provides an overview of different entitlements, eligibilities and notice periods in addition to whether leave can be delayed.
Junior Doctors’ Terms and Conditions of service
See Appendix VI for information on parental leave.
Bereavement-related leave
Support around Death
Though specific to those training within Scotland, this site aims to support all healthcare staff facing the death of a loved one. It offers information on the legislative, clinical and practical issues involved when balancing grief with training.
The following resources to support those on stress-related leave should also be consulted by those experiencing bereavement.
Stress-related Leave
The British Association for Counselling and Psychotherapy
If you believe more regular, face-to-face support might be best for you, this site is best able to signpost you to counselling and psychotherapy professionals within your area. When it comes to mental health, there really is no substitute for intensive, professional, one-to-one treatment.
DocHealth
This service offers face-to-face support from senior clinicians for those within the London area or skype consultations for those further afield. This service offers up to six sessions, though if further support is required, DocHealth will assist in finding you the best care possible. This service is exclusively by self-referral and, as such, shares no information with your employer. Fees are salary-dependent and services are set to expand within the coming year.
The Doctors’ Support Network
This site gives you access to a confidential peer support network for both doctors and medical students alike with concerns regarding their mental wellbeing. Beyond this, the DSN works to raise awareness and reduce stigma regarding mental illness amongst physicians.
Sickness-related Leave
NHS Practitioner Health Programme: Occupational Mental Health Services
This is an NHS service specifically for doctors (training and practicing) and dentists with both physical or mental health concerns that could affect their work. Though most suitable for those training within London, therapeutic services can be accessed externally (funding, via The Cameron Fund, may need to be applied for to do this).
Out Of Practice Research
BMA Guidance note on transferring between NHS and university employment during training
This resource provides detailed information on how best to tackle what can be a pretty jarring transition between clinical and academic life and back again. This includes a step-by-step guide on how to initiate, manage and, most importantly, enjoy your OOPR.
BMJ – Guide To Taking Time Out
This resource takes you through everything from how to make the best letter of application possible to the important differences between taking an OOPR within the UK and abroad.
BMJ – Research Options for Doctors In Training
This lists all research options currently open to trainee doctors and how you can maximise your chances of securing a place.
Out Of Practice Experience
The General Medical Council’s Guide to OOP for Doctors in Training
Given that all applications for time away must be directed to the GMC, knowing exactly what they’re looking for will put you in good stead for being approved. This website is essential reading for this.
London Paediatrics’ Guidance on OOPEs
This site provides a step-by-step breakdown of the application and selection process within any OOP experience that is relevant to any specialism.
Personal Accounts of OOPEs
This site provides a variety of OOPE case studies you may find helpful in planning your own time away. First-hand experiences here include time spent training in South Africa, New Zealand, Bangladesh and Australia. Click through for more general information provided by the Royal College of Emergency Medicine on all OOP opportunities available.
The British Medical Journal also includes a helpful blog on the OOPE, outlining pathways of application and potential difficulties whilst training. Click through.
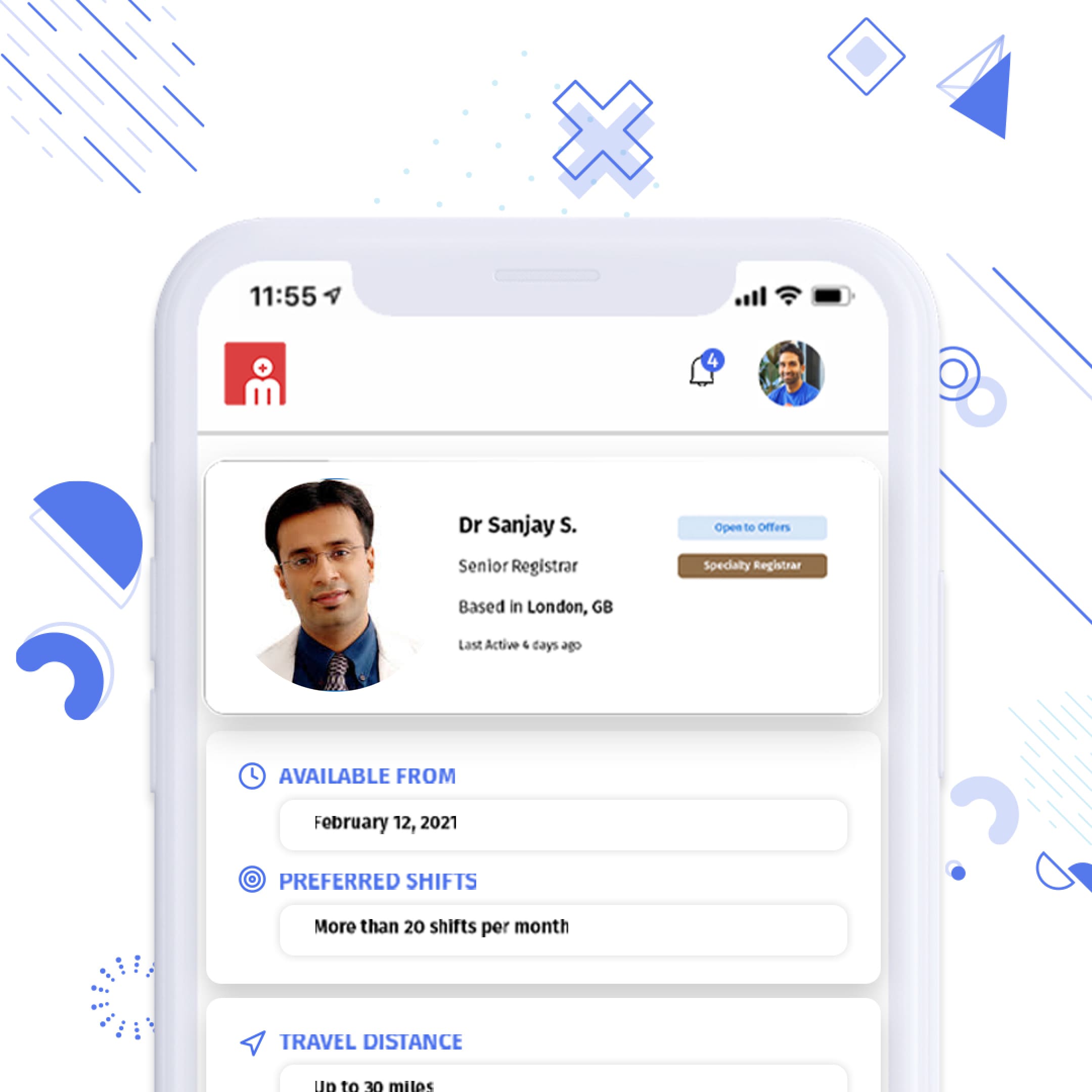
Find locum work on your terms
The best locum agencies together in one place, competing to find you the best locum shifts. Managed for free through your Messly account.